
In this 3-part series, we will discuss how implementing the AristaMD platform can support the transition to value-based care payment models.
- Part 1: How is the VBC payment model changing?
- Part 2: What challenges are driven by the value-based care transition?
- Part 3: eConsults for successful value-based care
With the transition to value-based health come challenges. Primary care practices, particularly smaller ones, must significantly upgrade their technology. Both to be sure that when they are referring a patient, the patient stays in-network and that the specialist is available to provide care. With the ongoing shortage of specialists, this remains a challenge.
Challenges to value-based healthcare typically fall into four categories:
- Interoperability
- Data & Workflow
- Financial Risk
Interoperability
Interoperability has been a challenge in healthcare for many years. To control costs under a value-based payment model PCPs must communicate the appropriate patient information when referring to a specialist to:
- Ensure that an appropriate diagnosis is made.
- Prevent duplication of diagnostics that increase the cost.
Unfortunately, most EHRs do not ‘talk’ to each other, and even when two providers are on the same EHR, the ability to share information between two practices is often difficult. Appointment scheduling platforms are not always connected to the practice’s EHR and are rarely connected to the scheduling platform of a specialist receiving a referral.
EHRs and scheduling systems don’t have all the information necessary to validate a patient’s health insurance to determine if prior authorization is required or which specialists are in-network for a particular patient’s health insurance.
Keeping patients in-network when referring to a specialist is critical to reducing the cost of care and ensuring those needing specialist advice attend the appointment. Tracking down this information often takes time. Time is the enemy of scheduling a referral. The longer it takes to schedule a referral, the more likely the patient is to:
- Seek an out-of-network provider.
- Fail to schedule the appointment.
- Select a high-cost alternative, like the ED.
As a result, the Archives of Internal Medicine reports that only about half of the referrals resulted in a completed visit to the specialist.
Data and workflow
Failing to schedule an appointment highlights the challenge of adapting the PCP workflow. PCP clinics often refer to local or familiar specialists. Referral coordinators rarely have visibility of the appointment wait times of in-network providers. When that information is available, the referral coordinator may still lack knowledge about distance or cost to the patient.
This transition also requires primary care clinics to collect patient data and track metrics demonstrating improved patient outcomes. The clinical workflow is often not designed to capture or monitor these metrics. Processes need to be defined to encourage patient utilization of preventative care, like notifications, follow-up phone calls related to preventive care or the completion of referrals, including receiving the diagnosis and treatment plan back from a specialist.
A study published in the Journal of General Internal Medicine reported that less than 35% of referrals resulted in closed-loop documentation – meaning that the referring provider received the information about the patient’s diagnosis and treatment from the specialist that provided care.
Common Value-based Healthcare Challenges
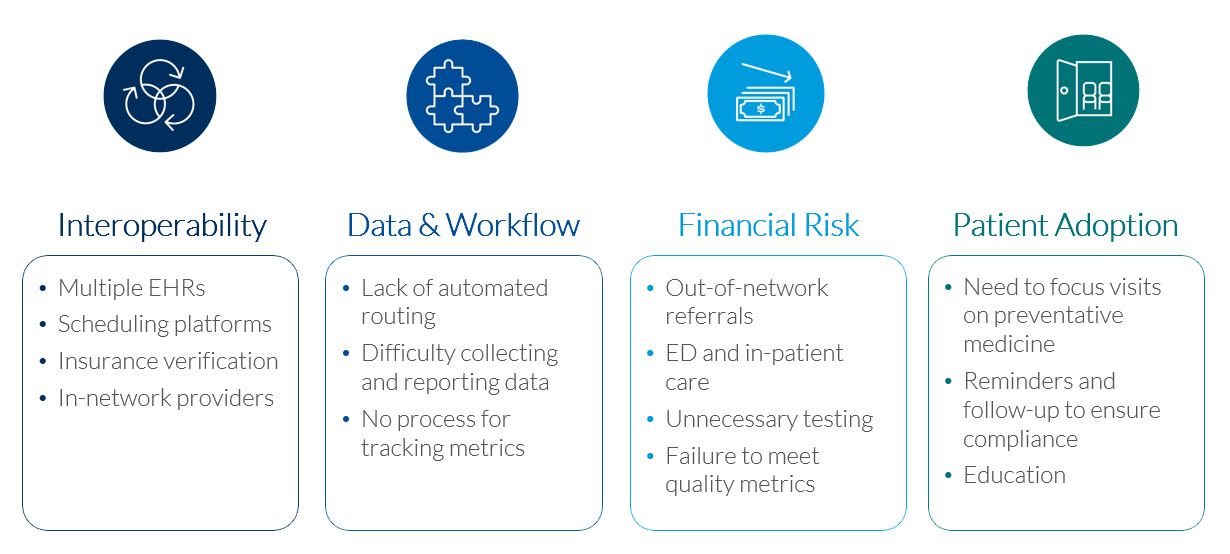
Financial risk
Closing the loop is essential to mitigating financial risk. Without confirmation that the patient scheduled the referral and received a diagnosis and treatment from the specialist, the primary care practice can assume that some patients are not receiving treatment. These patients are more likely to experience worsening symptoms – uncontrolled hypertension or unmanaged diabetes – that lead to expensive treatment, including ED visits and hospitalization.
In addition, PCPs who don’t receive feedback from the specialist about the referral’s outcome are unlikely to know who is responsible for follow-up care. Becker reported that 40% of patients who follow through with a referral never follow up with the referring physician after the care is initially provided.
Value-based care also pressures clinics to eliminate duplicate and unnecessary testing. Healthcare Finance News reports that unnecessary tests and treatments account for $200 billion in medical spending each year.
How do eConsults support value-based healthcare?
In the U.S., there are significant inequalities in specialty care access. Inequalities are worse when patients are:
- Minority
- Low-income status
- Speak limited English
- Reside in rural areas
Access concerns lead patients to seek care through alternate sites, like the ED, or forego appointments. In addition, primary care providers are often the best option for patients with limited ability to travel and concerns about copays and language barriers. Physicians have been seeking advice from their peers for centuries – in person, by letter and phone and now through our platform.
Before secure electronic communication was available, providers would consult a specialist by phone or in person. You often hear this referred to as a curbside consult because the complete patient history is rarely shared with the consulting specialist. If the PCP could not resolve the issue after speaking with a specialist, the PCP would transfer the care by referring the patient to a specialist.
eConsults combine these options by providing the specialist access to the patient’s medical history via secure, HIPAA-compliant access to the patient’s history and relevant imaging and lab work. Rather than transferring the patient’s care, the PCP receives advice from a specialist and provides care to the patient. An eConsult is an electronic request for advice from a specialist that precludes transfer of care – in most cases, the PCP provides care. Physicians have sought advice from their peers for centuries – first by letter and now through our platform. eConsults have the additional benefit of giving the specialist secure, HIPAA-compliant access to the patient’s history. Instead of consulting a specialist by phone, the PCP can send the information and receive a response in a few hours.
Historically, eConsults replace more than 70% of in-person visits. With longer appointment wait times due to COVID and specialist shortages, eConsults serve patients with more complex conditions. Despite the complexity, eConsults are replacing more than 74% of in-person visits year-to-date and influencing 92% of treatment plans developed by primary care providers using AristaMD.
