
In this 3-part series, we will discuss how implementing the AristaMD platform can support the transition to value-based care payment models.
- Part 1: How is the VBC payment model changing?
- Part 2: What challenges are driven by the value-based care transition?
- Part 3: eConsults for successful value-based care
How is the VBC payment model changing?
Value-based care is a trending topic and an industry buzzword. Value-based care payment models emphasize quality over quantity of care. Providers are rewarded for improving:
- Health outcomes
- Patient satisfaction
While CMS and other payers incentivize primary care providers to raise the overall quality of care by rewarding providers for efficiency and efficacy. The programs offer a few actionable steps to make value-based care a reality.
How can a provider tangibly deliver better, more efficient, and more effective care?
Truly, the answer is as simple as eConsults. eConsults are proven to save patients money and reduce the cost of care for both providers and payers.
eConsults serve as a preventive measure in specialist backlogs and worsened health outcomes resulting from delayed patient care. Additionally, eConsults improve the accessibility of quality care to those in lower-income, rural and other underserved areas.
What is value-based care?
While almost everyone working in healthcare today is familiar with the phrase “Value-based Care”, it’s important to articulate a common definition.
In 2006, Michael Porter and Elizabeth Teisberg explained the value equation as: Value equals quality divided by cost. This definition of value-based care has evolved from the Porter-Teisberg definition to describe the payment model or form of reimbursement which ties payment for care to the quality of care provided. This form of reimbursement has emerged as an alternative and potential replacement for fee-for-service reimbursement, which pays providers retrospectively for services delivered based on bill charges or annual fee schedules.
What is changing in value-based care?
With the passage of the Affordable Care Act (ACA), the first value-based care model was launched. The CMS Innovation Center was established by Congress in 2010 to identify ways to improve healthcare quality and reduce costs. The CMS Innovation Center develops and tests new healthcare payment and service delivery models to support five pillars of value-based care:
- Drive accountable care
- Advance health equity
- Support care innovation
- Address affordability
- Partner to achieve system transformation.
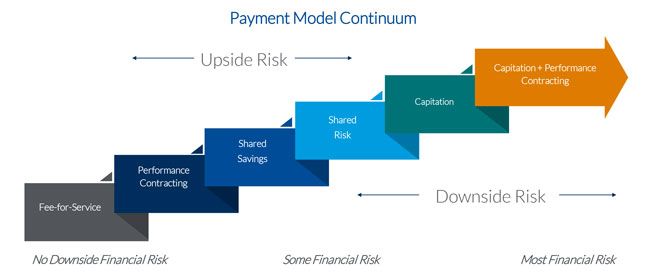
Since the ACA was passed, CMS has shifted payment to providers from fee-for-service to upside risk, and now, to more downside risk.
Upside financial risk means the provider is paid to care for a group of patients during a defined timeframe using the health status of the patients being served by that provider. If the provider can provide appropriate care for less than the contracted payment, the payer and provider share the savings. If the provider exceeds the pre-determined payment, there is no financial penalty.
Downside financial risk requires the provider to refund the payer if the actual cost of care exceeds a defined benchmark. Two-sided risk, or shared risk, combines both the upside and downside risk models.
Downside risk includes capitation, which is when a physician or group of physicians receives a risk-adjusted amount of money for each patient during a defined period, regardless of the number of patient visits, tests, or other services that would have generated a payment to the provider under a fee-for-service model.
What is driving the push toward downside risk?
CMS and commercial payers are limiting many value-based programs to encourage providers to assume more downside risk. A few headlines and upcoming changes to CMS payment models support this conclusion:
- CMS, HHS Finalize 2023 Notice of Benefits, Payment Parameters
- Accountable care models will be almost universal for Medicare and Medicaid beneficiaries by 2030, CMS leaders say
- State benchmarking programs can drive investments in primary care, Manatt report finds
CMS focuses on care delivery, reimbursement, and measurement of the advancement of health equity. All of these announcements highlight at least 1 of the 5 pillars of value-based care – accountable care, health equity, and innovation. HHS and CMS announced 2023 notice of benefits and payment parameters including Healthcare Marketplace plans that support health equity, patient outcomes, and gathering more robust data.
These recommendations require that Qualified Health Plans include healthcare disparities in their Quality Improvement Strategies and become accredited in health equity. This announcement also emphasized a great need for HHS is eager to develop a data-driven understanding of social determinants of health (SDOH) that improves clinical and non-clinical outcomes. In the NBPP, the agency requires plans to submit five new data variables while requesting input on broader SDOH data types, their value, collection barriers, and related incentives. Payer response to these five variables—ZIP code, race, ethnicity, and Individual Coverage Health Reimbursement Arrangement (HRA) and subsidy indicators.
Accountable care models will be almost universal for Medicare and Medicaid by 2030. In 2021, the Center for Medicare and Medicaid Innovation announced a plan to move Medicare beneficiaries and most Medicaid beneficiaries to coverage under an alternative payment model (APM) by 2030. Providers are getting a nudge toward value-based payment, but they will also receive more help transitioning to value-based payment, which often requires updates to technology as well as enhanced data and quality reporting.
CMS announced the ACO REACH Model that will replace the Global and Professional Direct Contracting Model, or GPDC Model. The goal of this change is to place a renewed focus on health equity and bring the benefits of value-based care to underserved communities. REACH will also emphasize provider-controlled governance and information monitoring – both are critical to managing value-based payment models. Finally, Fierce Healthcare reports states are directing healthcare spending toward services that support long-term population health, which is important to address affordability and achieve system transformation. Affordability and system transformation are also pillars of value-based care.
